Senescence and the search for anti-aging senolytics for Alzheimer’s disease
- Sasha Elizar, M.S.

- Jan 15, 2024
- 13 min read
Updated: Oct 7, 2025
Immortality is an alluring concept, especially when accompanied by the possibility of looking and functioning young. Now, it may be possible to increase the lifespan of humans by 20% in our lifetime. In pursuit of longevity and extending healthy years, scientists are investigating a process called senescence.
During senescence, cells stop dividing—they exit the cell cycle. This isn’t normally a problem for neurons, most of which are post-mitotic. The issue is that much like cancer cells, senescent cells are DNA damaged, death-resistant, metabolically active, rely more on the energy-inefficient process of glycolysis for energy, and are better able to withstand biological stress. These cells secrete pro-inflammatory signaling molecules (cytokines, chemokines, and extracellular matrix remodeling enzymes), which are collectively known as the senescence-associated secretory phenotype (SASP). SASP spreads pathology to neighboring cells, contributing to the aging process.
Ultimately, these “zombie cells” drive inflammation and many age-related diseases, earning them the designation as a hallmark of aging.
Senotherapeutics are a class of approaches that target senescent cells. They fall into two major categories: senomorphics and senolytics. Senomorphics suppress the SASP, essentially rendering senescent cells quiescent, whereas senolytics selectively clear senescent cells while sparing healthy cells. The mechanism by which senolytics target and eliminate senescent cells is still unclear.
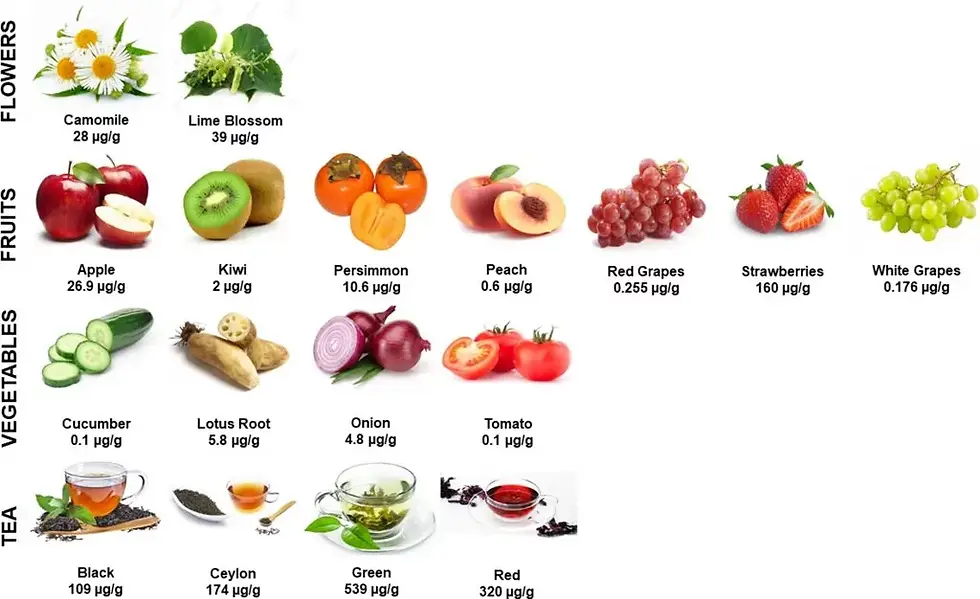
Fisetin, an antioxidant naturally found in strawberries and a variety of foods, joins quercetin and resveratrol as a molecule being investigated for its potential to treat dementia. Quercetin and resveratrol have already been found to act as senolytics in the brain. Fisetin, on the other hand, has been shown to be a senolytic in other tissue such as fat cells, but whether it can also clear aged brain cells remains unknown. It is able to pass the blood-brain barrier.
The search for senolytics for Alzheimer's disease
P301L mouse model of tauopathy in FTD
Flavonoids as senolytics in brain aging
Background
Epidemiology of Alzheimer's disease
Alzheimer’s disease (AD), the most common form of dementia, is a neurodegenerative disease that gradually leads to loss of memory, personality, and sense of self. This loss of selfhood is apparent in artist William Utermolen’s self-portraits.

As people live longer, AD rates are climbing steeply, which is expected to place a great burden on society in the coming years. It is the only leading cause of death with no established and widely-recognized prevention or treatment. Currently, the rates are highest in the southeastern and western United States.
In 2022, AD affected over 6 million Americans, killed 1 in 3 seniors, cost the nation $321 billion, and impacted over 11 million caregivers (Alzheimer’s Association, 2022). It is projected to cost the US over $1 trillion by 2050.

The National Institute on Aging (NIA) defines AD by neuropathology, particularly abnormal protein aggregates, including extracellular amyloid beta (Aβ) plaques and intracellular neurofibrillary tangles (NFTs) containing tau phosphorylated at multiple residues (p-tau). This neuropathology is confirmed via lumbar puncture for cerebrospinal fluid (CSF), blood, positron emission tomography (PET), or postmortem autopsy.
Neurodegeneration is the closest correlate of cognitive decline, which is marked by memory loss, inability to learn new information, and language difficulties. AD is also marked by brain atrophy, particularly in the hippocampus (in the temporal lobe), and enlarged ventricles.

Billions of dollars have been spent to immunologically clear Aβ plaques and tau tangles from the brain, but these drugs don't improve patients' symptoms much, don't slow down progression of the disease, and come with side effects. Importantly, diagnostic biomarkers don’t necessarily track with cognitive decline. Because high levels of Aβ and p-tau have been found in the brains of cognitively normal individuals, these proteins may not necessarily be the pathological drivers, necessitating a more nuanced approach that accounts for clinical heterogeneity.
A precision medicine approach to Alzheimer's disease: important considerations
Translating research in animal models into benefit for patients with AD will require understanding (1) brain region- and cell subtype-specific susceptibility to neurodegeneration, (2) the interactions of genetics, alternative splicing, and posttranslational modifications with longevity, and (3) divergent signatures of gene expression underlying different functional changes in different patients.
Neuronal subtypes are selectively vulnerable to neurodegeneration
Previous work by Leng and colleagues at UCSF has used single nucleus RNA sequencing (snRNAseq) to cluster cell subtypes in the entorhinal cortex (EC) and superior frontal gyrus (SFG) by gene expression markers and correlate them with Braak stages. Braak staging is a way to classify the degree of pathology in AD. They initially used well-known markers (like GAD for inhibitory neurons, AQP4 for astrocytes, MOG for oligodendrocytes) to generate heat maps of gene expression. Then, they performed functional network analysis (finds out which biochemical pathways are related) and pathway enrichment analysis (finds out which pathways are enriched in particular regions or cell subtypes). In this way, they discovered subtypes of excitatory neurons lost in these regions with increasing Braak stage (specifically in the EC and in L2 of the SFG). For instance, they found that the proportion of TBR+ (excitatory neuronal marker) cells decreased with increasing Braak stage. Furthermore, they found that the proportion of TBR+ cells that are also RORB+ (a subtype-specific excitatory neuronal marker, found to correlate with the phospho-tau marker CP13 across all Braak stages) decreased with increasing Braak stage, and that RORB+ expression was enriched in CP13+ cells at Braak stages 5-6. Their finding was consistent across multiple independent cohorts [1].
The observation of decreased excitatory neurons in the EC and the colocalization of p-tau with particular excitatory neuron subtypes, taken together, show that certain neurons are selectively vulnerable to neurodegeneration. This suggests that accounting for cell type specificity could help develop more effective and molecularly precise therapeutics.
Different rates of decline are driven by genotype, isoform, and posttranslational modifications
In addition, clinical heterogeneity is apparent with the simple observation that different AD patients are diagnosed at different ages and progress through disease at different rates. Dujardin and colleagues at Harvard Medical School have reported that some patients reach the maximum CDR-SOB (a measure of cognition and daily function in dementia) score in 6 years, and others in 17 years from diagnosis [2]. Some never reach the maximum score before death. This brings into focus the possibility of slowing disease progression and maximizing healthspan by investigating functional differences between patient populations and identifying therapeutic targets.
Tau is an important pathological biomarker in AD that accounts for biological variability. Tau is a natively unfolded protein that can take on six different alternatively spliced isoforms with different sites and amounts of phosphorylation. Depending on the sites on tau that are phosphorylated, conformational changes can occur with different rates of seeding, or proneness to aggregation. (Seeding is defined by the area that a specific protein species of interest takes up). Some conformations of tau have faster rates of aggregation, which are related to earlier age of onset and faster rates of disease progression. That is, certain forms of tau are "stickier" and "clumpier" than others, giving rise to more aggressive forms of disease.
AT8 is one such clinically established epitope of p-tau used to measure level of seeding. Neuropathologists look at AT8 for Braak staging in AD, which arises during an intermediate stage. It has been found that the higher the expression of AT8 p-tau, the faster disease progresses [2]. Importantly, tau seeding correlates with age of death (r = -0.51). Taken together, this suggests that tau species may influence longevity.
Divergent patterns of gene expression reveal disease subtypes
AD affects a wide variety of processes, accounting for clinical heterogeneity. Neff and colleagues at Icahn School of Medicine at Mount Sinai took parahippocampal RNAseq data and used clustering algorithms to generate AD subtypes, which they called A, B1, B2, C1, and C2 [3]. With this pipeline, they then used machine learning to predict AD subtypes with 83% accuracy. These subtypes have distinct molecular signatures, network regulator genes, and matched mouse models, and the subtypes were consistent across multiple cohorts. Type C was characterized as Aβ predominant, while types A and B were strongly linked to microtubule-associated protein tau (MAPT) activity. Type C exhibited downregulated excitatory synapses and synaptic signaling, an upregulated immune system / blood-brain barrier (BBB) and circulatory system, downregulated mitochondrial genes, decreased metabolism, and an increase in oligodendrocytes, astrocytes, oligodendrocyte precursor cells (OPCs), endothelial cells, and microglia. Meanwhile, type A showed upregulated excitatory synapses, a compromised immune system / BBB, upregulated protein degradation pathways (ubiquitination, proteasome), decreased myelin and OPCs, increased oxidative phosphorylation, increased catecholamine secretion, and downregulated microglial, endothelial, and astrocytic genes. Even though the same region was vulnerable—the hippocampus—it had the strongest subtyping signal over other regions. Overall, their findings suggest that AD subtypes may be split into those selectively vulnerable to synaptic depression (class C) or synaptic excitation (classes A and B).
The implications of these findings are dire. Opposing synaptic, glial, mitochondrial, metabolic, and immunological changes may be present in two different patients, increasing the risk that one may be harmed by an inappropriate medication. The authors suggest a hopeful future in which guess-and-test prescription is obsolete, and instead patient data is loaded into a database with multiple drugs tested in silico to see if they shift gene expression to a more favorable profile. They offer with optimism that this pipeline can also be used to accelerate identification of compounds that change levels of key regulator genes, which can be validated in clinically relevant animal models [3].
In summary, the characterization of various elements, including posttranslational modifications, brain regions and cell types involved, and gene expression signatures help to get a more granular picture of AD and pave the way for personalized medicine. The key takeaway is that a targeted molecular approach is needed to maximize health and lifespan in AD. Digital spatial profiling and other multi-omic approaches will become cornerstones of therapeutic research and development. Moving forward, it will be important to study the relation between tau and the aging process to prevent the onset or delay the progression of Alzheimer’s disease and promote healthy longevity.
Tau rTg(P301L)4510 mouse model of frontotemporal dementia
To study tau pathology, my graduate school lab used the transgenic rTg(P301L)4510 mouse model, which possesses doxycycline-repressible expression of mutant human tau. This P301L mouse model was developed and reported in 2005 by Santacruz, Ramsden, and colleagues [4, 5]. First, an “activator animal” contains a calcium-calmodulin kinase (CaMKII) promoter upstream of a tetracycline-off open reading frame containing the tetracycline transactivator (TTA) gene. In the absence of a tetracycline antibiotic, such as doxycycline, TTA is transcribed into protein. A second animal, the “responder animal,” contains a tetracycline-responsive element (TRE) upstream of human four-repeat tau with a P301L mutation in exon 10. When these animals are crossed, TTA binds the promoter of the responder cDNA that contains the TRE, transcribing the mutated tau. Because transgene expression is driven by the CaMKII promoter system, breeding the “activator animal” and the “responder animal” results in high levels of forebrain expression, primarily in neuronal cell types. All-in-all, human tau expression can be triggered by removing doxycycline at different stages in the offspring’s lifespan.
Ramsden’s group at the University of Minnesota looked at these mice’s tau tangles and found that, importantly, they get human tangles, they look like human tangles, and genetically they are human tangles. Further, transgenic human tau was expressed at a level 13 times higher than native mouse tau. Using in situ hybridization, they found tauP301L mRNA was largely restricted to the hippocampus, cortex, olfactory bulb, and striatum. NFT pathology started in the neocortex and progressed into the hippocampus and limbic structures with age, consistent with frontotemporal dementia (FTD).
Silver staining demonstrated a rapid onset of tau pathology around 2.5 months. From 4 months old, tauP301L mice had significantly lighter brains, severe cortical atrophy, and impaired spatial reference memory in the Morris water maze (MWM) task compared to littermate controls [5]. At 7 months old, rTg4510 mice were severely impaired with target quadrant occupancies indicating random swimming (25%). There was striking age-related neurodegeneration in CA1 of the hippocampus. NFTs occurred initially in CA1 pyramidal neurons, spread to CA2, and by 8.5 months of age included CA3 and the dentate gyrus.
Furthermore, Neff et al. collected RNAseq data from 19 mouse model studies, publicly available at the AMP-AD portal on synapse.org, and found the tauP301L mouse model is consistent with a tau-predominant class A subtype of AD. On the other hand, the 5XFAD model was found to match up most closely with the Aβ-predominant subtype C of AD [3]. Taken together, the rTg(P301L)4510 mouse is a clinically relevant model for tauopathy in AD and FTDP-17 (frontotemporal dementia) neurodegeneration, the condition linked to the P301L mutation.
Relation between senescence, inflammation, and tau

Tau pathology, as previously delineated, is related to the rate of decline and age of death in AD. Our lab investigates the causes and hallmarks of aging, and we are specifically interested in senescence in the brain and its link with tau. Senescence, a change in cell function, is an important process that occurs with aging. Senescent cells are metabolically active, demonstrate active DNA damage responses, rely on anti-apoptotic, pro-survival defenses to a greater extent than non-senescent cells, and are better able to withstand oxidative stress, giving them much in common with cancer cells. However, senescent cells are post-mitotic and do not divide. Additionally, senescent cells secrete inflammatory signaling molecules, collectively known as the senescence-associated secretory phenotype (SASP). In this manner, they spread pathology throughout the brain.
The interactions between senescence and tau aggregation were previously unknown. Dr. Miranda Orr’s group at University of Texas San Antonio performed an ingenuity pathway analysis (IPA) to look at differences in upstream regulators between AD patients with and without NFTs. They found pathways related to cell survival and tumor cell viability were greatly upregulated in AD patients with NFTs [6]. This suggests that senescence-associated pathways, like cell survival, regulate tau aggregation.
Orr and colleagues examined the predicted upstream regulators of tau tangles, and they found NF-kB, a pro-survival master transcription factor for inflammation characteristic of senescence. They also found enriched inflammatory cytokines and receptors, including IFN-γ, TNF, TLR4, IL1β, and CXCL1. This suggests that tau aggregation advances with inflammation.
Furthermore, the same analysis was applied to the P301L mice after the onset of NFTs comparing ages 6 months and 2 months. They saw inflammation upstream of senescence and NFTs. Similar to humans, upregulated cytokines included IFN-γ, TNF, and IL1β, further supporting the use of the mouse model for tau-associated senescence. Additionally, they quantified transcripts for p21 and p16 (senescence markers and cell cycle inhibitors) and found they were upregulated in the P301L model. This suggests that tau NFTs drive senescence as well. Finally, they quantified forebrain RNA expression of cytokines like Il1b, Tnfa, Cxcl1, and Tlr4 in 16- to 18-month-old mice and found that P301L mice had increased SASP. Altogether, tau NFTs may drive senescence and inflammation.
So far, we’ve learned that senescence and inflammation strongly drive tau aggregation, and that tau aggregation can drive further senescence and inflammation. Then, can we target AD-associated tau NFTs by inhibiting the continuation of the senescence phenotype? The most lasting way to intercept senescent cells in the brain that contribute to tau pathology and further senescence, and the approach we have chosen, is to selectively clear the cells with a class of therapeutics called senolytics.
Flavonoids as senolytics in brain aging
Yousefzadeh and colleagues at Scripps and Mayo Clinic screened a series of flavonoids and found that fisetin performed best at reducing senescent cell burden in a progeroid (Ercc1-/-) mouse model of accelerated aging, in a dose-dependent effect [7]. 20 μM fisetin decreased senescent murine embryonic fibroblasts (MEFs) by 50% in vitro. Furthermore, fisetin increases health and lifespan. Wild-type (WT) mice given fisetin starting at 20 months at a dose of 500 mg/kg lived significantly longer than control diet-fed mice, averaging an 11% increased lifespan. Fisetin also significantly decreased brain pathology and neuron loss, as determined by histopathological grading.

Possible mechanisms of action of fisetin include downregulating NF-kB and SASP (including IL1β), stimulating autophagic degradation of p-tau via TFEB (lysosome regulator), Nrf2 activation, inhibiting p38/MAPK (a kinase specific to serine and threonine and a pro-survival regulator of senescence-associated genes), PI3K/Akt/mTOR inhibition (which may in turn promote apoptosis), counteracting microgliosis, and activating mitophagy [8, 9]. How fisetin specifically selects senescent cells and how it moves through the body (pharmacokinetics) and is metabolized (pharmacodynamics) remain largely unknown. Additionally, how senescent cells are cleared from the brain once they are apoptosed by senolytics remains murky. They may be engulfed by microglia or washed out by the glymphatic system at night while we sleep, but the exact mechanism has yet to be elucidated.
In pursuit of senolytics for tauopathy
Dr. Miranda Orr is an Associate Professor of Gerontology and Geriatric Medicine at Wake Forest University School of Medicine. The Alzheimer’s Disease Drug Discovery Foundation awarded her team a three-year, $1M/year grant through February 2024 for SToMP-AD, a Phase II clinical trial to evaluate the safety and feasibility of senolytic therapy in Alzheimer’s disease. The major goal of this project is to gain data on the safety and efficacy of dasatinib and quercetin treatment on senescence, cognition, and tau pathology in older adults with mild cognitive impairment or early Alzheimer’s disease.
Her team is evaluating whether fisetin is a disease-modifying therapeutic. Through quantitative, histological, transcriptomic, and proteomic methods, her team hopes to answer whether fisetin influences age-related cell survival, p-tau NFT accumulation, and senescence in rTg(P301L)4510 mice. The behavioral arm of the study has been completed and experiments and data analysis are underway.
Dr. Miranda Orr's lab employs GeoMx digital spatial profiling, which is capable of simultaneously imaging over 1,000 transcripts and 100 proteins on the same tissue, including those involved in autophagy, glia, immune cells, cell death, and various p-tau species—S199, S396, T214, and T231—to give extraordinarily detailed location-based data on gene expression. This will help her team visualize the region-specific effects of fisetin in greater detail. In particular, Thr231/Ser235 (antibody: TG-3) displays high seeding and intense phosphorylation signal (r = 0.74) and serves as a clinically relevant intermediate marker for tauopathy [2, 5].
It will be important to look at region-specific effects (e.g., CA1, CA3, dentate gyrus) on senescence markers (e.g., p16, p19) due to the role of senescence in longevity and rate of tauopathy progression. Many questions remain, such as the functional involvement of microglia in tauopathy. Overall, her team is hopeful the project will reveal fruitful therapeutic targets.
Related Press
Additional Resource

References
Leng, K., et al., Molecular characterization of selectively vulnerable neurons in Alzheimer's disease. Nat Neurosci, 2021. 24(2): p. 276-287.
Dujardin, S., et al., Tau molecular diversity contributes to clinical heterogeneity in Alzheimer's disease. Nat Med, 2020. 26(8): p. 1256-1263.
Neff, R.A., et al., Molecular subtyping of Alzheimer's disease using RNA sequencing data reveals novel mechanisms and targets. Sci Adv, 2021. 7(2).
Santacruz, K., et al., Tau suppression in a neurodegenerative mouse model improves memory function. Science, 2005. 309(5733): p. 476-81.
Ramsden, M., et al., Age-dependent neurofibrillary tangle formation, neuron loss, and memory impairment in a mouse model of human tauopathy (P301L). J Neurosci, 2005. 25(46): p. 10637-47.
Musi, N., et al., Tau protein aggregation is associated with cellular senescence in the brain. Aging Cell, 2018. 17(6): p. e12840.
Yousefzadeh, M.J., et al., Fisetin is a senotherapeutic that extends health and lifespan. EBioMedicine, 2018. 36: p. 18-28.
Kim, S., et al., Fisetin stimulates autophagic degradation of phosphorylated tau via the activation of TFEB and Nrf2 transcription factors. Sci Rep, 2016. 6: p. 24933.
Ding, H., et al., Fisetin ameliorates cognitive impairment by activating mitophagy and suppressing neuroinflammation in rats with sepsis-associated encephalopathy. CNS Neurosci Ther, 2022. 28(2): p. 247-258.







Comments